
My name is Kathalina, and I have myasthenia gravis. I am 26 years old and am a registered nurse in the emergency department of my local hospital.
I have worked my way up to being a charge nurse, and I am proud of my accomplishments. I am also in graduate school to become a family nurse practitioner.
Aside from my professional career, I am married to my best friend; we have been together since high school and live with our golden retriever.
I’m telling you about my life and career so you can understand how myasthenia gravis has affected me. I was diagnosed in October 2023.
Although there is a lot more to know about myasthenia gravis, I’m not here to lecture on pathology; instead, I am just sharing my experience to raise awareness of the disease and its impact on one’s life.
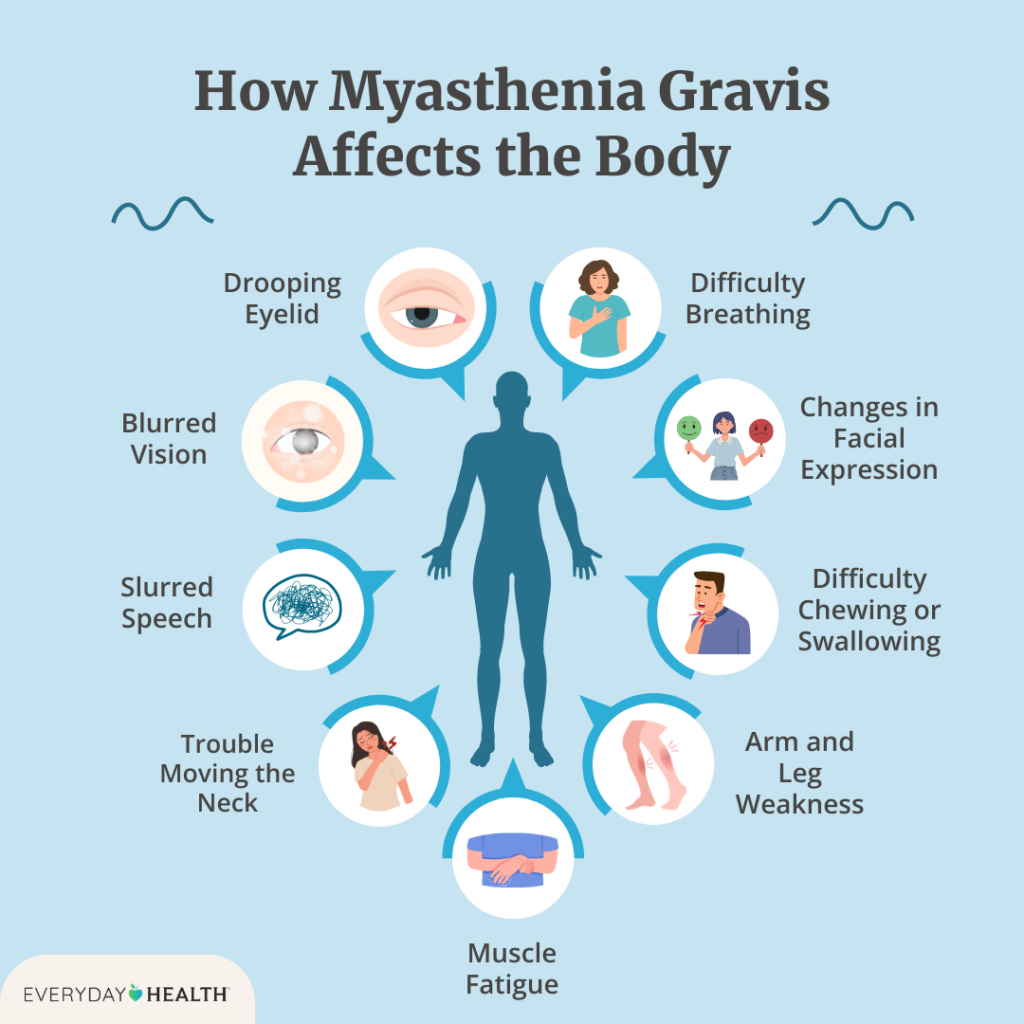
Symptoms
Let me take you to the very beginning, in May 2023, when my symptoms first started.
I remember this so vividly – my husband and I were on our way to my little brother’s high school graduation, and I remember looking at the mirror inside of his truck and smiling. Something about my smile was off, but I couldn’t quite put my finger on it. I turned to look at my husband, attempted to smile, and joked to him, “Am I having a stroke?”
We laughed it off and attributed it to me needing to wear my mouth retainer every night (I was terrible at wearing my retainer). Deep down, it made me feel insecure, but I brushed it off to focus on my family.
I now know that this was an early symptom of myasthenia gravis.
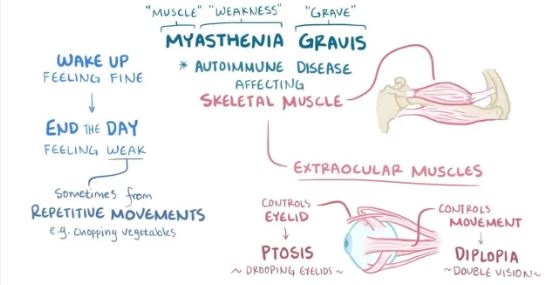
Early myasthenia gravis symptoms can be very subtle, right? Another symptom I had was dysarthria, which means trouble forming words. One night I was making macaroni and cheese for dinner, and I couldn’t say “cheese” clearly. Dysarthria can be caused by muscle weakness and can occur when consonants are not pronounced correctly.
As a nurse, these symptoms reminded me of a stroke. I was starting to worry, so I finally decided to reach out to my primary care doctor.
My primary care doctor was unsure what it could be. I was a healthy 26-year-old, no medical history, no medications. I got an MRI scan, which came back normal. I was not having as much slurred speech, but my smile was still off. It made me want to cry, and I started to feel very insecure about myself.
I continued my pace of working 12-hour shifts and going to graduate school. I had a lot on my plate, but I thought I could handle it.
Four months after symptoms began, in October 2023, I was on my way to work when I started to have double vision (diplopia) and a droopy eyelid (ptosis). The double vision got so bad that I had to pull over on the side of the road. This freaked me out, and I remember calling my husband and my mom, who thought it was anxiety. I thought maybe it was a problem with my new glasses, so I scheduled an appointment with the optometrist the next day I was off work.
At work, I stare at a computer screen for almost 12 hours. I remember having vision changes and feeling like my eyelid was so heavy. I asked the emergency room doctors and nurse practitioners I work with what they thought was wrong. We were all leaning towards Bell’s Palsy, which made sense at the time because I was under a lot of stress.
Diagnosis
My optometrist referred me to an ophthalmologist, who wanted to do blood work to rule out the “big and scary stuff like myasthenia gravis” – that’s word for word what he said in the appointment.
“Myasthenia Gravis?” I thought to myself. I haven’t heard of that since nursing school! Honestly, I thought the ophthalmologist was grasping at straws.
But then, a week later (yes, it took that long to get the lab results back), I opened my phone and saw all the lab results in red. I cried and cried for hours as I wondered what this meant for me.
I remember Googling “myasthenia gravis: autoimmune, chronic, no cure,” a myriad of thoughts running through my head as I scrolled page after page, story after story.
The labs that my ophthalmologist ordered were:
- Acetylcholine receptor binding antibody, reference range is positive > or =0.50 nmol/L, mine was 29.08 nmol/L.
- Acetylcholine receptor modulating antibody, reference range <32 inhibition, mine was 91% inhibition.
- Acetylcholine receptor blocking antibody, reference range <15% inhibition, mine was 59% inhibition.
I immediately sent a copy of these lab results to my primary care doctor and made an appointment with him the next day. With these lab results and my symptoms, he diagnosed me with myasthenia gravis.
He started me on Mestinon, ordered a CT of my chest to rule out thymoma, and referred me to a neuromuscular specialist. I began to do a lot of research on who I would want as a neuromuscular specialist. It was important for me to have someone who would understand me and my goals.
I also began to experience weakness in my arms and hands, to the point that brushing my hair or brushing my teeth became exhausting. I could not even put my hair up in a towel with my own hands. Being unable to perform even simple, daily tasks was getting to me, and I was so frustrated and depressed by my new “normal.” I did not want to be around anyone or be out in public because I was so ashamed of myself and my struggles.
Next Steps
Many factors can make myasthenia gravis worse, including stress, anxiety, fatigue, lack of sleep, overexertion, extreme temperatures, humidity, and sunlight. I was pushing myself at work and in school, which added a lot of stress to my life.
Being diagnosed with myasthenia gravis made me realize I needed to take a step back to focus on my health. Ultimately, I made the decision to prioritize my well-being.
I got a new job on a day-shift schedule closer to home. I also decided to take a few semesters off from school. That was tough, as it felt like I was giving up on something for which I had worked so hard. It upset me to quit until I realized that I wasn’t “giving up” – I was doing what was best for me.
Meanwhile, Mestinon was helping with my symptoms, but I had to take it every four hours. If I didn’t, my symptoms would come back very quickly.
I was feeling a little bit better, but still not like myself.
I kept thinking, is this my new normal? Is this how I am always going to feel? It brought me into a deep depression as I reflected on my old life, just a year ago, when I was symptom free.
In February 2024, my neuromuscular specialist invited me to participate in a clinical trial. I decided that was my best option.
The trial, sponsored by Regeneron Pharmaceuticals, is evaluating an experimental combination treatment with pozelimab and cemdisiran, and cemdisiran monotherapy. As part of Phase 1, I have a monthly subcutaneous injection in the abdomen and, at each visit, there are assessments and strength testing to see how I am doing.
As I write this, it has been four months since I joined the trial, and my symptoms have been reduced almost 95%. I am feeling like my old self.
Don’t get me wrong – I still have days where I need to take Mestinon or I need to rest because I can feel my eyelid drooping or my arms starting to become weak. But this treatment plan has allowed me to continue doing what I love – working as an emergency room nurse, spending time with my family, traveling, and being able to confidently smile in pictures. I will also be returning to school to complete my family nurse practitioner degree in the fall.
Being able to take part in this research trial fills me with gratitude and makes me optimistic. There are many treatment options out there – you just have to find the right one for you, even if it takes some trial and error. Never lose hope.
With my background in nursing, I want to continue to learn more about myasthenia gravis and educate myself and others about it. I firmly believe that participation in clinical trials can advance myasthenia gravis research in significant ways.
I am not saying that this clinical trial will be a cure, but it sure has allowed me to continue living my life and, for that, I am eternally grateful.


